Negative Thought Patterns Schizophrenia way authorized to reproduce or copy both a completed paper (essay, term paper, research paper coursework, dissertation, others) or specific Negative Thought Patterns Schizophrenia parts of it without proper referencing. The Company is not responsible and will not report to any third parties due to unauthorized utilization of its /10() Apr 28, · It's fairly common for people with schizophrenia to have trouble keeping their thoughts straight and expressing what's in their minds. Disorganized thinking is one of the primary symptoms of schizophrenia, and it can lead to a variety of thought process disorders that cause disjointed thoughts, a collapse or sudden stop in thought process, randomly spoken words, Estimated Reading Time: 8 mins Sep 11, · a free revision, if Negative Thought Patterns Schizophrenia there are only slight inconsistencies in your order. Your writer will make the Negative Thought Patterns Schizophrenia necessary amendments free of charge. You Negative Thought Patterns Schizophrenia can find out more information by visiting our revision policy and money-back /10()
Negative Symptoms of Schizophrenia: Understanding Them - Living With Schizophrenia
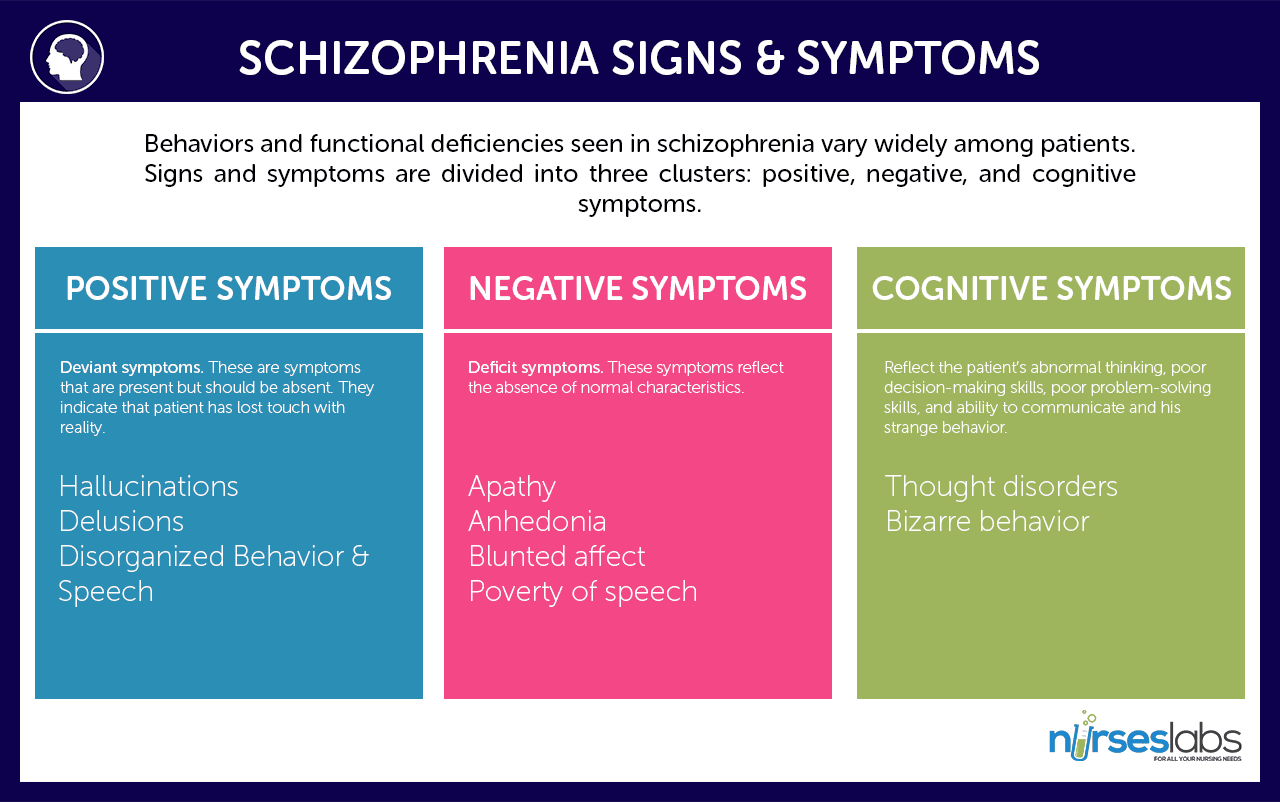
Try out PMC Labs and tell us what you think. Learn More. Schizophrenia is frequently a chronic and disabling disorder, characterized by heterogeneous positive and negative symptom constellations. The objective of this review was to provide information that may be useful for clinicians treating patients with negative symptoms of schizophrenia.
Negative symptoms are a core component of schizophrenia that account for a large part of the long-term disability and poor functional outcomes in patients with the disorder. The negative symptom domain consists of five key constructs: blunted affect, alogia reduction in quantity of words spokenavolition reduced goal-directed activity due to decreased motivationnegative thought patterns schizophrenia, and anhedonia reduced experience of pleasure, negative thought patterns schizophrenia.
Negative symptoms can occur at any point in the course of illness, although they are reported as the most common first symptom of schizophrenia. Negative symptoms can be primary symptoms, which are intrinsic to the underlying pathophysiology of schizophrenia, negative thought patterns schizophrenia, or secondary symptoms that are related to psychiatric or medical comorbidities, adverse effects of treatment, or environmental factors.
While secondary negative symptoms can improve as a consequence of treatment to improve symptoms in other domains ie, positive symptoms, depressive symptoms or extrapyramidal symptomsprimary negative symptoms generally do not respond well to currently available antipsychotic treatment with dopamine D 2 antagonists or partial D 2 agonists.
Since some patients may lack insight about the presence of negative symptoms, these are generally not the reason that patients seek clinical care, and clinicians should be especially vigilant for their presence. Negative symptoms clearly constitute an unmet medical need in schizophrenia, and new and effective treatments are urgently needed.
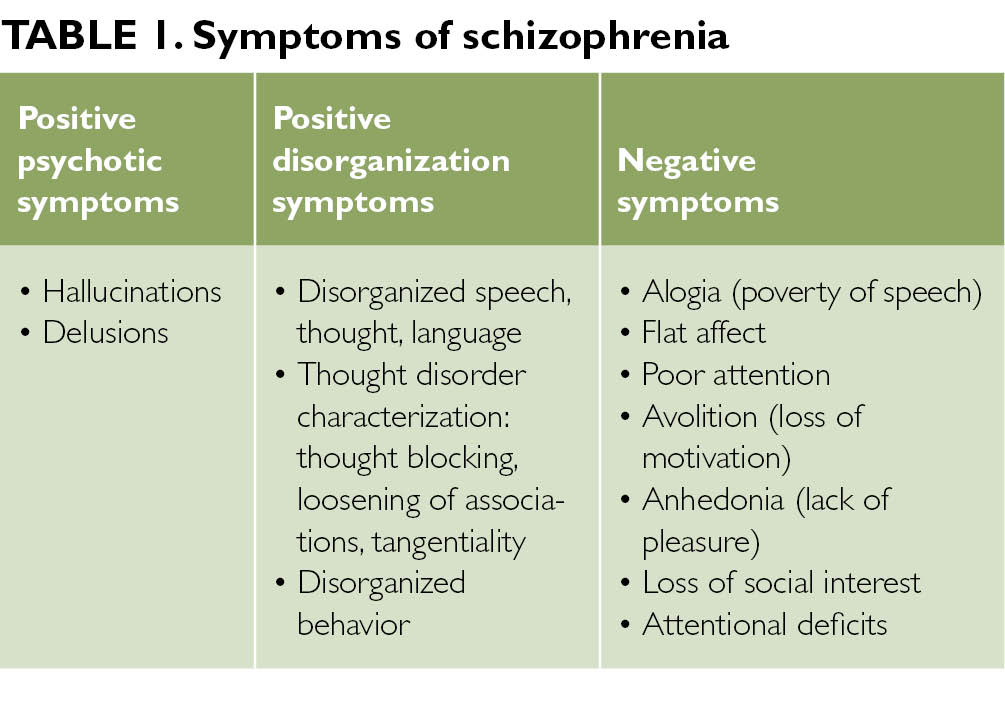
While positive symptoms reflect an excess or distortion of normal function eg, delusions, hallucinations, disorganized behaviornegative symptoms refer to a diminution or absence of normal negative thought patterns schizophrenia related to motivation negative thought patterns schizophrenia interest eg, negative thought patterns schizophrenia, avolition, anhedonia, asociality or expression eg, blunted affect, alogia.
Negative symptoms are a core component of schizophrenia and they account for a large part of the long-term morbidity and poor functional outcome in patients with the disorder. Although positive symptoms are generally effectively managed with available antipsychotic medications, limited treatment options are available for negative symptoms and despite advances in understanding the epidemiology, etiology, negative thought patterns schizophrenia, biology, and psychopharmacology of schizophrenia, they remain an unmet medical need.
The objective of this narrative review is to provide clinicians with a comprehensive source of information about the diverse attributes of negative symptoms of schizophrenia. This current information about the anatomy, assessment, and management of negative thought patterns schizophrenia symptoms aims to be useful to clinicians treating patients with this challenging manifestation of schizophrenia.
Reference databases were searched to identify articles relevant to our topic. This search retrieved entries. We narrowed our results by searching in conjunction with more specific terms, such as definition, assessment, symptom domains, factors, secondary negative symptoms, functional impairment, and treatment. Additionally, reference lists of relevant reviews and primary studies were manually searched to find articles that did not appear in our computerized search.
English language articles that were published in peer-reviewed journals were included. The content of the search results was divided into the following sections: Terminology, Course, Prevalence, Burden, Neurobiology, Clinical Presentation, Assessment, Treatment, and Best Clinical Practices. Although some negative symptoms are signs that can be observed by a clinician eg, affective flattening, alogiaother aspects of behavior, such as social withdrawal or diminished engagement in productive or pleasurable activities, may or may not be associated with negative symptoms.
As such, asking patients about their interests, emotions, and motivation adds great value to patient observation during negative symptom assessment. Although various more specific terms are used in the literature to describe the nature and etiology of negative symptoms eg, deficit, predominant, negative thought patterns schizophrenia, prominent, persistent as they pertain to research, there is no consensus definition for any term Table 1.
Differentiating primary negative symptoms intrinsic to the underlying pathophysiology of schizophrenia from secondary negative symptoms related to other factors can be challenging, negative thought patterns schizophrenia. Secondary symptoms, which can respond to treatment, occur in association with or result from positive symptoms, negative thought patterns schizophrenia, affective symptoms, medication side effects, environmental deprivation, negative thought patterns schizophrenia, or other treatment- or illness-related factors Figure 1.
Although several negative thought patterns schizophrenia have demonstrated negative symptom improvement in clinical trials that were designed to study patients with acute exacerbation of schizophrenia defined by positive symptoms, treatment response should not be inferred in this context since secondary negative symptoms can improve as a consequence of improvement in other symptom domains.
While the distinction between primary and secondary negative symptoms is important for researchers and clinical trial design, negative thought patterns schizophrenia symptoms can be difficult to differentiate.
As such, the clinical focus should be on managing all negative symptoms that affect patients, do not respond to the current treatment, persist during periods of clinical stability, and interfere with normal role functions.
From this viewpoint, clinicians can appreciate that any patient with a clinically significant level of negative symptoms, either alone ie, predominant negative symptoms or concurrently with positive symptoms ie, prominent negative symptomscan benefit from appropriate clinical management. Negative symptoms have been reported as among the most negative thought patterns schizophrenia first symptom of schizophrenia, 9 although they generally do not represent the reason that clinical care is initially sought for patients.
Genetic contributions, prenatal events, and poor premorbid adjustment may all contribute to the development and evolution of early negative symptoms in psychotic illnesses. Negative symptoms commonly appear during the prodromal phase of schizophrenia and before the first acute psychotic episode Figure 2.
Schematic course of negative symptoms in schizophrenia. Negative symptoms are present throughout the course of schizophrenia.
They can occur early, persist over time, increase in severity, and remain between acute episodes of illness. Correll, C. The Prevalence of Negative Symptoms in Schizophrenia and Their Impact on Patient Functioning and Course of Illness.
The Journal of Clinical Psychiatry. CopyrightPhysicians Postgraduate Press. Reprinted by permission. The long-term course of negative symptoms is unclear, with some studies reporting relative stability of symptoms over time, and others finding that negative symptoms could fluctuate or be reversible. Evidence consistently supports the concept that negative symptoms constitute a distinct group of symptoms in schizophrenia that are separate from positive symptoms, depression and anxiety, and disorganized thought, speech, and behavior; higher prevalence of negative symptoms is noted among men, the unemployed, and in individuals with reduced functioning.
Compared with positive symptoms, which can be managed in many patients with currently available dopamine D 2 partial agonists and antagonists, negative symptoms have a higher burden of illness.
This pronounced illness burden can be attributed to negative thought patterns schizophrenia limited number of effective and evidence-based treatment options, although underrecognition of these symptoms also plays a role. It is very important to assess and address negative symptoms in an effort to lessen the associated burden on patients, caregivers, and healthcare systems.
Negative symptom severity in schizophrenia has been consistently linked to worse functional outcomes in areas such as impaired occupational and academic performance, negative thought patterns schizophrenia, household integration, negative thought patterns schizophrenia, social functioning, participation in activities, and quality of life.
Although affective symptoms may appear to be anhedonic in nature, individuals with schizophrenia seem to be able to experience consummatory pleasure, with functional decline specifically related to the inability to anticipate pleasure in pursuing or achieving goal-directed behavior. Negative symptoms negative thought patterns schizophrenia schizophrenia are likely to be the result of irregularities of distributed neural networks eg, frontocortico-temporal, cortico-striatalas opposed to negative thought patterns schizophrenia disruption of any discrete region of the brain.
The dopaminergic hypothesis of schizophrenia proposes that positive symptoms are the result of hyperactivity of dopaminergic neurotransmission in limbic pathways, while negative symptoms, loss of motivation, negative thought patterns schizophrenia, and impairment in cognition are thought to arise from hypodopaminergic functioning in the frontal lobe and additional mesolimbic structures. Due to their localization in mesolimbic regions of the brain that control reward, emotion, and motivation, dopamine D 3 receptors may also play a role in the modulation of negative symptoms, mood, and cognition.
As such, negative thought patterns schizophrenia, D 3 antagonists and partial agonists may provide benefits in negative or cognitive symptoms. Alternatives to the dopamine hypothesis suggest that other neurotransmitters, particularly glutamate, contribute to the development of symptoms in schizophrenia. The glutamate hypothesis is based on the clinical observation that chronic blockade of glutamate neurotransmission by antagonists at the N-methyl-D-aspartate NMDA receptor subtype eg, ketamine, negative thought patterns schizophrenia, phencyclidine produces a pathophysiological state resembling schizophrenia, including both positive and negative symptoms whereas the dopamine model of amphetamine-induced psychosis only produces positive symptoms.
Additional mechanisms of action, including metabotropic glutamatergic receptor mGluR2 agonism, alpha-7 nicotinic receptor agonism, and central nervous system stimulant activity, are also targets for drug development in negative symptoms of schizophrenia. Of note, however, the dopamine and glutamate hypotheses of schizophrenia are not mutually exclusive, with evidence in the literature supporting a role for both in the neurobiology of negative thought patterns schizophrenia. Indirect clinical evidence suggests an important interaction between dopamine receptors and NMDA receptors in critical brain regions, such as the hippocampus, and between glutamatergic afferents and subcortical dopaminergic nuclei.
It is generally accepted that negative symptoms include 5 key constructs, 61 which can be further categorized into 2 independent factors Figure 3. Key negative symptom constructs. Although the presence of negative symptoms is not mandatory for a diagnosis of schizophrenia, negative symptoms ie, diminished emotional expression and avolitionare 1 of the 5 symptom criteria taken into consideration in the Diagnostic and Statistical Manual of Mental Disorders DSM A level of functioning in work, school, relationships, or self-care that is markedly below the level that has previously been achieved is also diagnostic and suggests the presence of avolition and the reduced drive to pursue goal-directed behavior.
Clinical recognition of negative symptoms is challenging because patients with schizophrenia may not be aware of the impact of negative symptoms and they rarely present with negative symptom complaints. Furthermore, while clinicians have been well trained to assess and treat positive symptoms of schizophrenia, many are unsure of the best way to identify and treat negative symptoms. When seeing a patient with schizophrenia, clinicians should be on the lookout for a general presentation that suggests the presence of negative symptoms, including signs such as communication difficulties, flat affect, limited emotion, social inactivity, low motivation, and retarded psychomotor activity Figure 4.
While s ome of these problems are observable during clinical assessment, others need to be elicited through questions and discussions with the patient, family members, and caregivers, making informant input critical to the accurate assessment of the presence, severity, and impact of negative symptoms. Several validated and well-established assessment tools, such as the Positive and Negative Syndrome Scale PANSS65 the Scale for the Assessment of Negative Symptoms SANS66 and the item Negative Symptom Assessment NSA 67 are available to evaluate negative symptoms and track their course over time.
Of note, these scales only measure negative symptoms at a single timepoint and may be limited by the inclusion of items that are no longer considered relevant to the negative symptom domain eg, difficulties in abstract and stereotyped thinking, inattentiveness, negative thought patterns schizophrenia.
Newer scales that have been developed include the Clinical Assessment Interview for Negative Symptoms CAINS68 which covers all 5 negative symptom domains, negative thought patterns schizophrenia, and the Brief Negative Symptom Scale Negative thought patterns schizophrenia. None of these scales consider whether symptoms are primary or secondary to another aspect of illness, and administration may be limited by time constraints negative thought patterns schizophrenia the availability of trained raters.
Given the challenges associated with negative symptoms in the clinic, an easy-to-use instrument for rapid screening and assessment can benefit clinicians, patients, and families alike. One such tool is the NSA-4, 71 a condensed version of the NSA that rates behavior, not psychopathology; due to its focus and brevity, it is much more scalable and usable in busy clinical contexts.
The NSA-4 consists of 4 verbatim items from the full rating scale restricted speech quantity, reduced emotion, reduced social drive, negative thought patterns schizophrenia reduced interests and a global rating of the overall impression of negative symptom severity. Timely and successful assessment and management of negative symptoms are critical aspects of good patient care.
Since some patients may have limited self-awareness of negative symptoms as a part of their illness, clinicians must rely on observations during the interview, input received from informants, and information collected through revealing questions.
Careful assessment of patient responses to questions can help determine if a diagnosis other than negative symptoms is applicable or may rule out other conditions eg, comorbid depression that are common in people with schizophrenia-spectrum disorders.
Questions should be phrased to elicit broad responses in order to demonstrate whether a patient is able to elaborate on a response without prompting, participates in enjoyable activities to assess for anhedonia, has social contacts to assess social drive, and is goal oriented and productive.
Additional examples of questions that can elicit informative responses include: How do you spend a typical day? What do you do for fun? Have you had a chance to meet up with people outside of your family recently? and Would you like to have a job? For patients with more severe negative symptoms, some fundamental signs can be identified solely by observation of behaviors, such as poor grooming and hygiene, and reduced or impoverished content of speech. In the future, data collected through digital technology, such as smartphone applications, are expected to become increasingly available and used to enhance various aspects of patient assessment and care in the management of schizophrenia generally negative thought patterns schizophrenia negative symptoms in particular.
Although negative symptoms are classically described in relationship to schizophrenia, they also occur in other illnesses. While being aware that negative symptoms can be intrinsic to schizophrenia or related to an underlying cause is important, differentiating between them can be difficult, if not impossible. As such, clinicians should be vigilant for all clinically relevant negative symptoms in order to manage them properly and improve patient outcomes. Clinicians can provide the most appropriate treatment for each patient by observing their behavior, questioning them and their family members or friends, administering a formal assessment such as the NSA-4, considering differential medical diagnoses, and addressing factors that are associated with secondary negative symptoms.
Few studies have been prospectively designed to assess the effect of treatment on persistent negative symptoms, with most reports of improvement in negative symptoms being based on short-term studies in patients with acute psychotic illness and concurrent negative symptoms.
Moreover, superiority in regard to negative symptom improvement was also accompanied by negative thought patterns schizophrenia advantages for cariprazine over risperidone on the Clinical Global Impressions-Improvement Scale 85 and the Personal and Social Performance Scale, 86 indicating that the improvement of the negative symptoms with cariprazine additionally led to clinically meaningful advantages.
Beyond antipsychotic monotherapy, other drugs have also been used adjunctively with antipsychotics for the treatment of negative symptoms. Several trials have shown modest efficacy for adjunctive antidepressants, and limited evidence against negative symptoms exists for other adjunctive agents including glutamatergic compounds eg, glycine, D-serine, D-cycloserineminocycline, dopamine agonists eg, selegiline, modafiniland cholinergics eg, galantamine, donepezil.
Given the considerable unmet medical need associated with negative symptoms, drug development is active in this therapeutic area for agents with activity at different receptors including NMDA receptors, alpha 7 nicotinic receptors, 87 and 5-HT 2A and sigma-2 receptors. Moreover, it is still unclear how many patients with schizophrenia will remain stable on MIN while being off directly dopamine modulating medications and whether ongoing Phase 3 trials will replicate its negative symptom advantage, which was partly due to a rarely observed absence of negative symptom improvement on placebo.
Further, meta-analyses have shown that antidepressants may potentially be beneficial in treating negative symptoms. Moreover, the quality of some of the meta-analyzed studies may have been problematic, which further confounds the overall outcomes. Additionally, some medical devices, using approaches such as deep transcranial magnetic stimulation and transcranial direct current stimulation, are also under investigation for the negative thought patterns schizophrenia of negative symptoms.
Given the limited effective pharmacologic interventions to treat patients with negative symptoms of schizophrenia, it is important that clinicians are aware of psychosocial interventions that can be used in conjunction with antipsychotics.
Several psychological variables, including defeatist beliefs, negative expectations, and asocial preferences, are associated with negative symptoms.
General behavioral interventions, including a focus on healthy lifestyles, with emphasis on exercise, sleep, diet, smoking cessation, appropriate alcohol consumption, and social participation, should always be suggested in the course of treatment.
Thought Disorders: Different Types \u0026 Diagnoses – Psychiatry - Lecturio
, time: 7:29Thinking Process Abnormalities in Schizophrenia
Negative Thought Patterns Schizophrenia way authorized to reproduce or copy both a completed paper (essay, term paper, research paper coursework, dissertation, others) or specific Negative Thought Patterns Schizophrenia parts of it without proper referencing. The Company is not responsible and will not report to any third parties due to unauthorized utilization of its /10() Feb 21, · Evidence consistently supports the concept that negative symptoms constitute a distinct group of symptoms in schizophrenia that are separate from positive symptoms, depression and anxiety, and disorganized thought, speech, and behavior; higher prevalence of negative symptoms is noted among men, the unemployed, and in individuals with reduced functioning. 3, 6 Although negative symptom Cited by: 69 Jul 15, · Concrete thinking has been contended to be associated with schizophrenia, and divergent thinking is apparent in those who are schizophrenic. Robert Unger () can be paraphrased as stating that
No comments:
Post a Comment